The Function Of Peyer's Patches
Peyer's patches are oval-shaped areas of thickened tissue that are embedded in the mucus-secreting lining of the small intestine of humans and other animals. They were first observed by their namesake, Johann Peyer, in 1677. Although he was able to observe them using the technology available to him hundreds of years ago, they are known to be difficult to visualize because of the nature of their tissue structure and how they seem to blend into the surrounding intestinal lining. They are mostly concentrated in the ileum, which is the last section of the small intestine in humans before the large intestines begin. Even though Peyer's patches are a feature that can only be found in the gastrointestinal tract, their primary function is to operate as part of the immune system. The patches consist of lymphoid tissue; this means, in part, that they are full of white blood cells that are on the lookout for pathogens that might be mixed in with the digested food passing through the intestine.
TL;DR (Too Long; Didn't Read)
Peyer's patches are round, thickened areas of tissue located in the mucosa of the intestinal lining. Inside of the patch are a cluster of lymph nodules, filled with white blood cells. The surface epithelium of Peyer's patches is overlaid with specialized cells called M cells. The patches' morphology allows them to use a kind of isolated immune system to identify and target pathogens without involving the body's full immune response to every foreign body that passes through the intestines, including food particles.
An Isolated Immune System
An Isolated Immune System
The immune system is present and active throughout the body, although it takes different forms in different organs. It has three primary roles:
- Get rid of dead cells.
- Destroy cells growing out of control before they become cancerous.
- Protect the body from pathogens, such as infectious agents and toxins.
The gastrointestinal tract is exposed to an especially high number of pathogens that gain entry to the body by stowing away in foods and liquids. Therefore, it is important for the immune system to have a way to identify and target micro-organisms and other toxins that make their way into the gut. The problem is that if the adaptive immune system had as much of a presence in the lining of the small intestine as it does in the bloodstream and certain other tissues, it would be treating every food particle as a foreign body and a threat. The body would be in a constant state of inflammation and sickness because of the immune response, and it would be impossible to eat food or receive nutrients and hydration. Peyer's patches offer a solution to that problem.
Lymphoid Tissue Networks
Lymphoid Tissue Networks
Peyer's patches are composed of lymphoid tissue, including lymph nodules. Their composition is similar to the tissue in the spleen and in other parts of the body that are involved in the lymphatic system. Lymphoid tissue contains a large number of white blood cells. This kind of tissue is very involved in the immune system. Mucus-secreting membranes in the body are often part of the primary defense against pathogens. The innate immune system involves physical barriers, considered primary defenses, that act as the first blockade to keep out or remove pathogens. For example, the mucosal lining of the nostrils traps allergens and infectious microbes before they can gain further entry into the body. Lymphoid tissue is prevalent in mucosal areas, and supports their immune responses to foreign bodies with a secondary response called the adaptive immune system. The networks of lymphoid patches in mucosal tissue are known as mucosa-associated lymphoid tissues, or MALT. They provide the quickest and most precise adaptive response to pathogens.
Like the lining of the nostrils, the lining of the gastrointestinal tract is a mucus membrane that has early contact with foreign bodies. Food, drink, particles in the air, and other matter enter the body directly through the mouth. Peyer's patches are part of the network of lymphoid tissue located in the small intestine, along with additional lymphoid nodules that are scattered throughout the ileum, jejunum and duodenum. These nodules are similar in cellular morphology to Peyer's patches, but they are significantly smaller. This intestinal tissue network is a type of MALT and is also known more specifically as the gut-associated lymphoid tissues, or GALT. The patches' morphology (their shape and structure) allows them to use a kind of isolated immune system to identify and target pathogens without involving the body's full immune response to every foreign body that passes through the intestines, including food particles.
The Structure and Number of Peyer's Patches
The Structure and Number of Peyer's Patches
On average, each adult has 30 to 40 Peyer's patches in the organs of the small intestine. They are mostly in the ileum, with some in the adjoining jejunum and a few extending as far as the duodenum. Research has indicated that number of Peyer's patches present in the intestines drops off significantly after humans age past their late 20s. To find out how many Peyer's patches humans have when they are born and as they grow, scientists performed biopsies of the small intestines in infants and children of varying ages who had died suddenly of causes unrelated to the gastrointestinal tract. The results revealed that the number of patches increased from an average of 59 in third trimester fetuses to an average of 239 in adolescents in stages of puberty. The patches also increased in size during this time. For adults, the number of patches decreases with age beginning in the 30s.
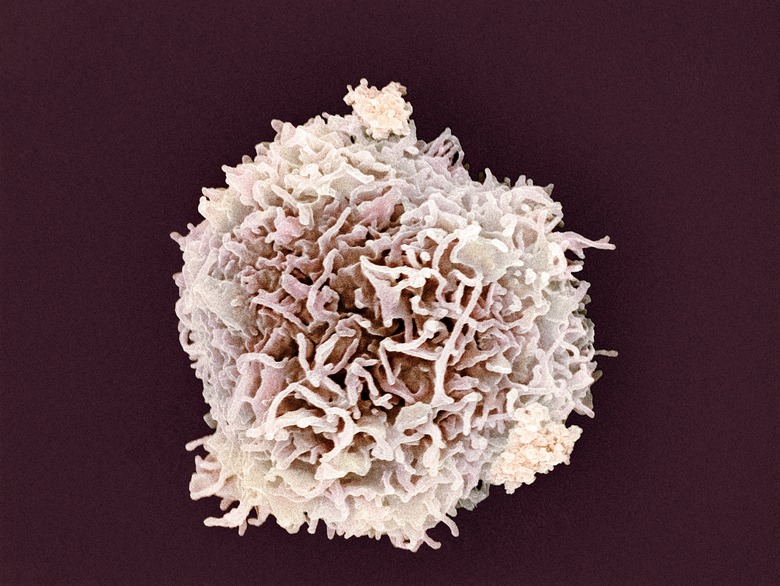
Peyer's patches are located in the mucosa of the intestinal lining, and they extend into the submucosa. The submucosa is a thin layer of tissue that connects the mucosa to the thick, tubular muscle layer of the intestines. Peyer's patches create a slight rounding in the surface of the mucosal lining, which extends into the intestinal lumen. The lumen is the "empty" space inside of the gastrointestinal tube, through which ingested matter passes. Inside of the patch are a cluster of lymph nodules, filled with white blood cells, especially ones known as B lymphocytes or B cells. Lining the domed surface of the patch in the intestinal lumen is the epithelium – a layer of cells that form a membrane over many organs and other structures in the bodies of animals. Skin is a kind of epithelium called epidermis.
The Brush Border and Surface Area
The Brush Border and Surface Area
Most of the cells lining the small intestine, which are called enterocytes, have very different morphologies compared to the epithelial cells on Peyer's patches. In the human body, the small intestine is looped around itself and some internal organs so much that if you were to straighten it out, it would measure about 20 feet in length. If the lumenal surface (the lumen is the inside of the tube, along which digested food matter passes) were as smooth as a metal pipe, its surface area would only measure approximately 5 square feet if flattened out. The enterocytes of the small intestine have a unique feature, however. The surface area of the small intestine actually measures about 2,700 square feet, which is approximately the size of a tennis court. This is because a lot of surface area has been scrunched into a small space.
Digestion does not only happen in the stomach. Many of the small molecules from food continue to be digested by enzymes as they pass through the small intestine, and this requires far more surface area than could fit in the intestine if it were a straight path from the stomach to the small intestine, or even if it followed the coiled path but the lining were smooth. The mucosal lining of the small intestine is rippled throughout with villi, which are countless projections into the lumenal space. They provide an increased surface area for enzymatic digestion of small molecules such as amino acids, monosaccharides and lipids. There is another feature of the intestinal lining that increases the surface area for digestive purposes. The enterocytes in the mucosal epithelium have a unique structure on the surface of their cells that face toward the lumen. Similar to the villi of the mucosa itself, the cells have microvilli, which as the word implies, are microscopic, densely packed projections extending into the lumenal space from the plasma membranes. When magnified, the microvilli look similar to the bristles of a brush; as a result, the length of microvilli, encompassing multitudes of epithelial cells, is called the brush border.
Peyer's Patches and Microfold Cells
Peyer's Patches and Microfold Cells
The brush border is partially interrupted where it meets Peyer's patches. The surface epithelium of Peyer's patches is overlaid with specialized cells called M cells. They are also known as microfold cells. M cells are very smooth compared to enterocytes; they do have microvilli, but the projections are shorter and are distributed sparsely across the lumenal surface of the cell. On either side of each M cell is a deep well called a crypt, and below each cell is a large pocket containing a few different types of immune cells. These include B cells and T cells, which are different kinds of lymphocytes, or white blood cells. White blood cells are an major part of the immune system. There are also antigen-presenting cells in the pocket beneath each M cell. An antigen-presenting cell is a category of cell that operates like a role in a play: It can be performed by a number of different cells in the immune system. One kind of immune cell that plays the role of antigen-presenting cell and can be found beneath the surface of an M cell is the dendritic cell. Dendritic cells have multiple functions, including destroying pathogens by a process called phagocytosis. This involves engulfing the pathogen and breaking it down into its parts.
M Cells Facilitate an Adaptive Immune Response
M Cells Facilitate an Adaptive Immune Response
Antigens are molecules that can potentially cause harm to the body, and activate the immune system to initiate a reaction. They are typically called pathogens until they have triggered the immune system and a protective response, at which point they earn the name antigens. M cells are specialized to detect antigens in the small intestine. Most immune cells that work to detect antigens look for "non-self" molecules or cells, which are pathogens that do not belong in the body. M cells cannot work by reacting to any non-self antigens they encounter the way other detector cells do, since M cells encounter so much non-self digested food material in the small intestine every day. They are specialized instead to react only to infectious agents, such as bacteria and viruses, as well as to toxins.
When an M cell does encounter an antigen, it uses a process called endocytosis to engulf the threatening agent, and transport it across the plasma membrane to the pocket in the mucosa where the immune cells are waiting. It presents the antigen to the B cells and dendritic cells. This is when they take on the role of antigen-presenting cells, by taking up relevant pieces of the broken-down antigen and presenting it to the T cells and B cells. Both the B cells and T cells can use the fragment from the antigen to build a specific antibody with a receptor that binds to the antigen perfectly. It can also bind to other, identical antigens in the body. The B cells and T cells release a number of antibodies with this receptor into the intestinal lumen. The antibodies then track down all of the antigen of this type that they can find, bind to them and use destroy them using phagocytosis. This usually happens without the human or other animal having any symptoms or signs of illness.
Cite This Article
MLA
E., Rebecca. "The Function Of Peyer's Patches" sciencing.com, https://www.sciencing.com/function-peyers-patches-7384313/. 31 August 2018.
APA
E., Rebecca. (2018, August 31). The Function Of Peyer's Patches. sciencing.com. Retrieved from https://www.sciencing.com/function-peyers-patches-7384313/
Chicago
E., Rebecca. The Function Of Peyer's Patches last modified March 24, 2022. https://www.sciencing.com/function-peyers-patches-7384313/