Antibiotic Resistance: Definition, Causes & Examples
Bacteria are found everywhere around the world, from arid deserts to moist caverns and dark forests. They can adapt to many environments and are found in particularly high numbers in and around many animals, including humans. Most of these bacteria are harmless, but there are many different kinds and large numbers of each kind.
Many bacteria are found in places such as on human skin and in the human digestive system. These bacteria help keep the skin smooth and pliant, and the gut bacteria help humans digest their food. These are the beneficial bacteria that evolved with humans and fulfill various functions for the human body.
What Do Harmful Bacteria Cause?
What Do Harmful Bacteria Cause?
While most bacteria don't cause any problems, a few are harmful and can cause a variety of infectious diseases. **Bacterial diseases** such as pneumonia used to be a serious threat and often caused death. In addition to disease, bacteria can also cause infections of cuts, wounds and in any other situation in which bacteria can enter the body through a break in the skin.
Infections were at one time a serious problem, and people could lose limbs or die. Bacterial diseases and infections became much less deadly with the discovery of the first antibiotic, penicillin, in 1928.
How Are Antibiotics Used?
How Are Antibiotics Used?
Antibiotics came into common use by the 1940s. In addition to penicillin, many other antibiotic drugs have been discovered. They have the same bacterial fighting effect as penicillin but work in various ways.
Today, antibiotics are widely used to cure bacterial diseases and infections but also to prevent sickness in farm animals. Their use in human health care and agriculture has led bacteria to develop resistant strains of bacteria that cause antibiotic-resistant infections.
Antibiotics are not effective against such bacteria, and when people and animals get sick from strains of resistant bacteria, their cure becomes increasingly difficult. At the moment some bacteria have become resistant to some antibiotics, but there are a few strains of antibiotic resistant bacteria that don't respond to treatment with any antimicrobial drug.
Treating infectious diseases and disease control in general becomes a serious problem if such drug-resistant bacteria become common.
What Exactly Are Antibiotics?
What Exactly Are Antibiotics?
Antibiotics are drugs that cure bacterial infections. They work by stopping bacteria from multiplying or by killing them. Some antibiotics only work against some types of bacteria, but broad spectrum antibiotics prevent the growth of many types of bacteria.
For the development of new antibiotics, scientists test many different substances for the ability to control bacterial growth and for side effects in humans. Some substances kill bacteria but are not safe to use. The testing and approval process is so long that only a few antibiotics make it through into common use.
How Do Antibiotics Work?
How Do Antibiotics Work?
Antibiotics disrupt some part of the bacteria's life cycle so that the bacteria die off and the infection disappears. Penicillin and other early antibiotics attacked a bacterium's ability to build and repair its cell wall. Unlike human cells found inside the body, bacteria have to be able to exist in the open environment and need a cell wall to protect them and keep the cell intact.
The penicillin type of antibiotic blocks the bacterial cell from linking molecules together to form its wall. When the cell wall deteriorates, the bacterium bursts and dies.
Other antibiotics that kill bacteria attack the bacteria's ability to produce proteins in their ribosomes. Since cells need proteins to function, the bacteria that are prevented from making proteins can't survive.
Another type of antibiotic prevents the bacteria from reproducing. Bacteria multiply by making a copy of the DNA in the cell and then splitting. The antibiotics disrupt the DNA copying process by breaking the strands of DNA into pieces and preventing the cell from making repairs.
Without a DNA copy, the bacteria can't split, or if it splits, the daughter cells can't survive. Using these types of antibiotics, health professionals have been able to cure bacterial infections and diseases quickly and easily until now.
What Is Antibiotic Resistance?
What Is Antibiotic Resistance?
Antibiotic resistance is the development of bacterial mechanisms that defeat the disruptive effects of antibiotics. As a result, antibiotics that used to cure specific diseases by preventing the growth of the associated bacteria no longer work. Such drug resistance becomes common as more and more bacteria change.
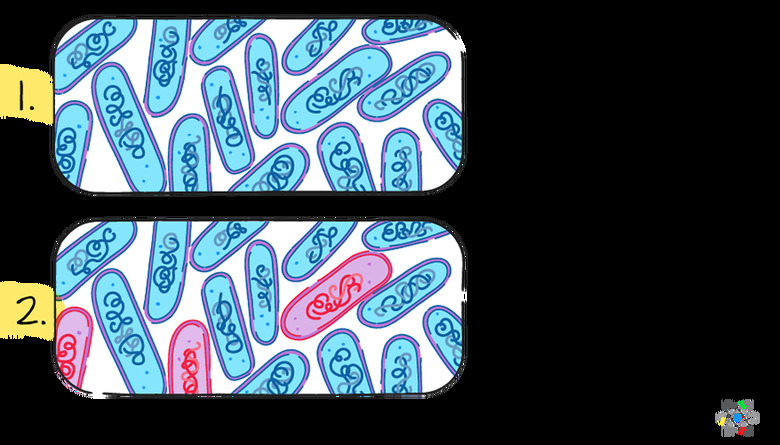
Even when only a few of the bacteria are resistant to the antibiotic used, the non-resistant bacteria are killed off while the remaining ones multiply to continue causing the disease. When this happens repeatedly, the resistant bacteria become more common, and more cases of antibiotic failure occur.
This is the situation at present. If the trend continues, eventually most bacteria will be resistant, and antibiotics will no longer be effective for disease control and prevention.
For example, several kinds of bacteria cause pneumonia, and the type of antibiotic that breaks up bacterial DNA strands to prevent the bacteria from splitting is often used to control and cure the disease. For antibiotic resistant bacteria, these antibiotics can no longer break up the DNA strands.
How Do Bacteria Keep Antibiotics from Working?
How Do Bacteria Keep Antibiotics from Working?
Bacteria have evolved special strategies to counteract the effects of antibiotics. Some bacterial cells have changed their cell wall to prevent the antibiotic from entering. Others pump the antibiotic out before it can do any damage. Still others attack and change the antibiotic so it no longer works.
Basically, individual bacteria have tried all kinds of strategies to survive, and some have found that mechanisms like these work to make them resistant to specific antibiotics. Bacteria may incorporate several of these methods to target antibiotics that work in different ways.
Some bacteria have many of these methods and are resistant to almost all antibiotics.
How Do Resistant Bacteria Spread?
How Do Resistant Bacteria Spread?
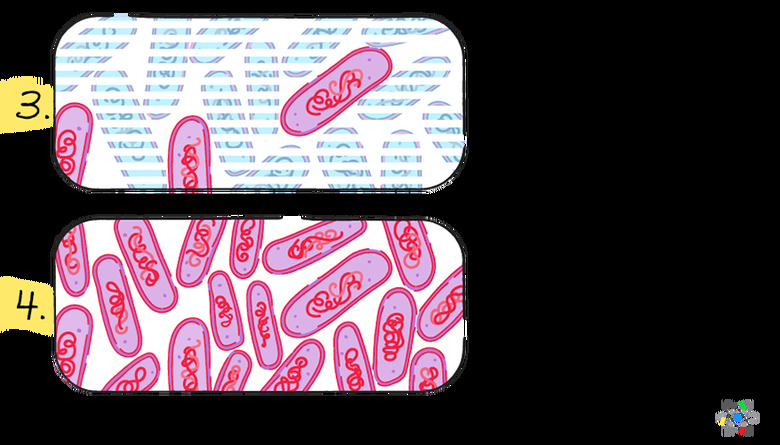
Once a bacterium has developed a resistance mechanism, it survives the antibiotic while all the other bacteria die. The process of curing disease with antibiotics results in a very strong selection pressure in favor of antibiotic resistance. Only resistant cells survive. They can then multiply rapidly and spread the resistance.
This means the resistant bacteria are automatically selected to become more common. If the sick patient or animal dies or when their bodily waste is discarded, these resistant bacteria are released into the environment where they can spread the resistant genes to other bacteria.
How Do Bacteria Develop Resistance?
How Do Bacteria Develop Resistance?
One way bacteria can develop mechanisms to defeat antibiotics is through **random mutations**. Although such a mutation may take place in only one bacterial cell, the strong selection pressure allows the resistant mutation to spread quickly. The resistant bacteria are the ones that survive and multiply and that then share the new resistant genes.
When an antibiotic is used at low levels for an extended period, bacteria have lots of time to mutate and for a mutation to spread. The longer an antibiotic is used in a certain situation, the more chance there is for mutations and for bacterial resistance to develop.
What Contributes to Antibiotic Resistance
What Contributes to Antibiotic Resistance
While random genetic mutations are the original source of antibiotic resistance, other factors have to be present and contribute to making the bacterial resistance into a serious problem.
Incomplete courses of antibiotic treatment and long-term antibiotic use can contribute to the development of resistant cells. Once a bacterial cell has the resistant mutation, fast asexual reproduction through bacterial cells splitting and multiplying can increase the number of bacteria that are resistant very quickly.
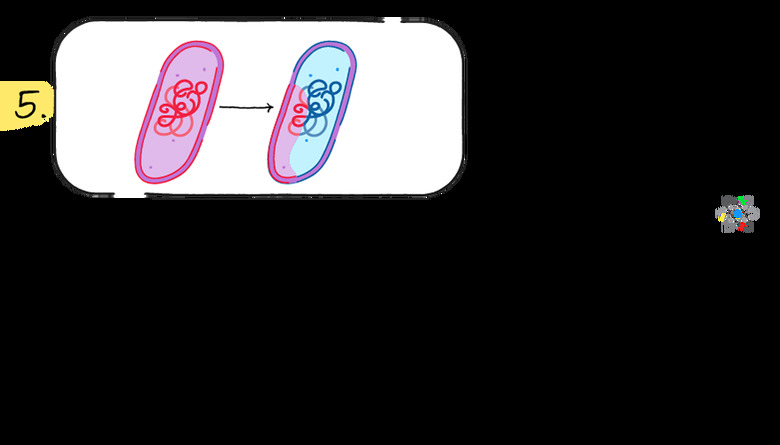
In addition to multiplying through cell splitting, bacteria have another mechanism for spreading the mutant and resistant genes. **Horizontal gene transfer** places copies of DNA fragments, possibly including resistant genes, into new cells.
DNA fragments in the form of plasmids can exist outside cells and can enter new cells, transferring DNA segments and genes without reproduction. This means resistant genes can jump between species or bacteria types as long as they come into close proximity.
Because a course of treatment with antibiotics basically has to kill every disease-causing bacterial cell to be sure that no resistant cell survives, it becomes important that antibiotic treatment in humans is always carried out to completion.
In practice, some bacteria not killed by the antibiotic may be killed by the natural immune system, but when a course of antibiotic treatment is not completed, and not all the doses are taken, the risk of survival of a resistant bacterial cell increases.
How Long-Term Antibiotic Use Is a Problem
How Long-Term Antibiotic Use Is a Problem
Long-term use of antibiotics, for example in hospitals, can increase the spread of resistant bacteria. Long-term use creates a permanent stage for strong selection pressure. Where a normal course of treatment may take two weeks during which selection pressure is applied and bacteria may mutate, long-term use is a continuous opportunity for random mutations.
Once a bacterium has developed antibiotic resistance, the ongoing use of antibiotics allows the bacterium to multiply and develop additional resistant mechanisms. Overuse of antibiotics has the same effect.
Whenever antibiotic use is frequent or spread over an extended period, the risk of spreading antibiotic resistance increases. This is especially true now that resistant genes are becoming more common.
The Effect of Long-Term Antibiotic Use in Agriculture
The Effect of Long-Term Antibiotic Use in Agriculture
A major factor in the development and the spread of antibiotic resistance is the use of antibiotics in agriculture.
Herd animals are highly susceptible to infectious diseases, and farmers counter the risk by feeding animals low levels of antibiotics to protect them. This constant use of antibiotics results in ideal conditions for the development and spreading of resistant mutant genes.
Although some of the antibiotics used in agriculture are not used in humans, horizontal gene transfer has allowed resistant agriculture genes to appear in antibiotics used in human treatments. Unless the use of antibiotics is drastically curtailed everywhere, including in agriculture, more and more antibiotic drug types will lose most of their effectiveness.
Why Is Antibiotic Resistance a Problem?
Why Is Antibiotic Resistance a Problem?
When antibiotic resistance spreads, the antibiotics currently in use become less effective. Bacterial strains causing disease in specific patients may have a varying degree of resistance to different antibiotics, and treatment could be delayed until an antibiotic that works is identified.
In the worst case, none of the available antibiotics works, and the patient's own immune system may not be able to fight off the bacteria. The patient becomes a source of antibiotic resistant bacteria that can spread throughout the hospital.
Because antibiotics work using several different means of disrupting bacterial functions, most bacteria develop resistance to one of these mechanisms but can still be killed off using other antibiotics that work differently.
The emergence of so-called "super bugs" is a serious problem because they have developed resistance to all known antibiotics. In those cases, only completely new antibiotics that employ new strategies will work, but such new drugs can't be developed quickly.
At the moment, bacteria are winning the race by developing resistance to existing antibiotics faster than new ones are discovered. If present trends continue, the time when no antibiotic works against some common diseases is not far away. Diseases that are easily cured today, may become deadly.
Why New Antibiotics Can't Solve the Problem
Why New Antibiotics Can't Solve the Problem
Antibiotics attack the way bacteria function, such as interfering with cell wall construction or with DNA. There are a limited number of ways bacteria can be attacked, and when the existing attacks no longer work, a completely new type of antibiotic is required that uses a completely new strategy.
There is no such antibiotic in existence at the moment, and those in development have not been approved as safe or as effective. Health care professionals are facing a future where antibiotics only work in a limited number of cases.
Why We Need to Reduce the Use of Antibiotics
Why We Need to Reduce the Use of Antibiotics
In addition to developing new drugs, a strategy of limiting the use of antibiotics to cases where they're really needed could help delay the further development of bacterial resistance. Often, when common infections are not serious, and the patient is healthy, the immune system can take care of and neutralize the bacteria.
In agriculture, raising healthy animals in a clean environment using disease-reducing practices can minimize the use of antibiotics and cut down on opportunities for the selection and spread of resistant bacteria. Health professionals and research scientists are using a two-pronged approach. Limiting the use of antibiotics in general and quickly looking for new types of antibiotics is the best way to keeping everyone healthy in the future.
Cite This Article
MLA
Markgraf, Bert. "Antibiotic Resistance: Definition, Causes & Examples" sciencing.com, https://www.sciencing.com/antibiotic-resistance-definition-causes-examples-13718429/. 9 July 2019.
APA
Markgraf, Bert. (2019, July 9). Antibiotic Resistance: Definition, Causes & Examples. sciencing.com. Retrieved from https://www.sciencing.com/antibiotic-resistance-definition-causes-examples-13718429/
Chicago
Markgraf, Bert. Antibiotic Resistance: Definition, Causes & Examples last modified March 24, 2022. https://www.sciencing.com/antibiotic-resistance-definition-causes-examples-13718429/